The thought of becoming a parent is associated with a lot of powerful emotions. The birth of a baby is expected to bring unmatched joy and contentment. But, sometimes, it may result in an unexpected condition that can hamper the growth of the child – Postpartum Depression.
Also referred to as Postnatal Depression, this condition is the onset of a depressed mood and its associated symptoms within the first year of childbirth. Although most mothers experience baby blues, some mothers develop persistent, severe symptoms that do not resolve.
Postpartum Blues and Postpartum Depression are two different expressions of the same issue, but Postpartum Depression is a long-lasting condition that should not be overlooked. Postpartum Blues, also known as Baby Blues, are temporary changes in mental and emotional state that occur in the mother within 2 to 3 days after childbirth and typically last for approximately 2 weeks.
They usually resolve on their own without requiring medical intervention. However, if the symptoms of Baby Blues intensify and persist for more than a couple of weeks, it is classified as Postpartum Depression (PPD), a more serious condition.
37-year Rebecca, mother to a four-year-old remembers experiencing irritability, sleep disturbances, stress, and anger after childbirth. She did not have a formal diagnosis, and prefers to associate her symptoms with “Baby Blues” and not “Postpartum Depression”, considering the severity of her condition.
It is important to seek treatment for postpartum depression, as it adversely affects the mother and the baby, and can disrupt the relationships shared amongst family members. With the right treatment, a woman can alleviate her postpartum depression symptoms and embrace motherhood by bonding well with her baby.
Postpartum Depression Causes
Postpartum depression (PPD) is caused by a combination of various factors, including emotional, environmental, biological, hormonal, and genetic influences. During the post-birth period, women undergo significant hormonal changes that leave them susceptible to depression. The reproductive hormones experience a sharp increase before delivery and then rapidly decline after, leading to an imbalance that can manifest as depressive symptoms.
Contributing factors to PPD include emotional issues within relationships or family dynamics, lack of support in caring for the newborn, young maternal age, low income, and immigrant status. Complications and stressful events during pregnancy and childbirth, a family history of depression, limited knowledge about PPD, acceptance of misconceptions, inadequate maternal care, and lack of sleep are also known causes of PPD.
Every year, there are 140 million births worldwide, while the prevalence of postpartum depression is estimated to be around 10–13 percent of new mothers. The obvious question is why some mothers get postpartum depression and not others.
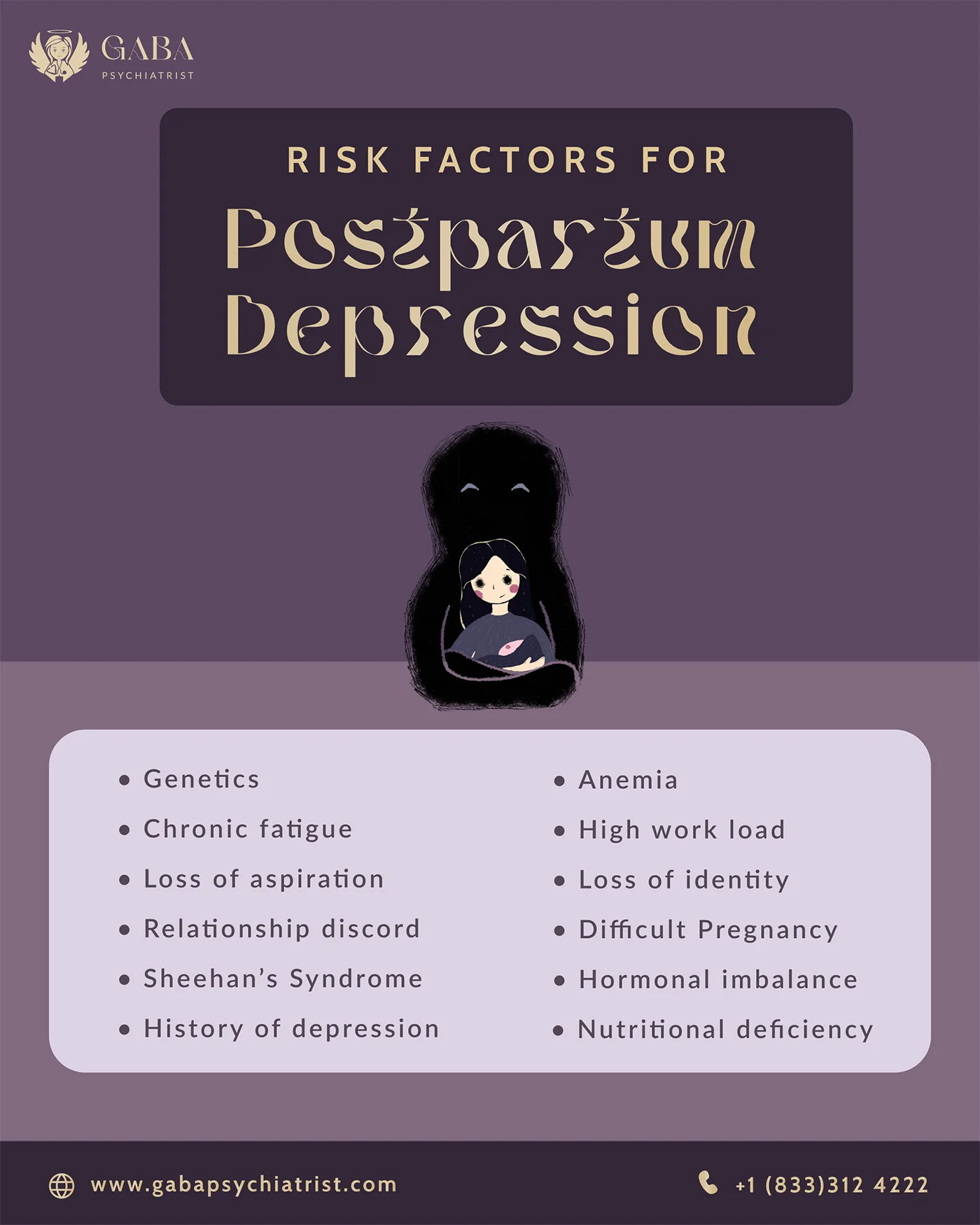
Risk Factors for Postpartum Depression
Are some women at a higher risk of developing postpartum depression than others? The answer is yes. New mothers may be relatively more prone to PPD if they:
- Had suffered from depression before or during pregnancy
- Experienced abuse as a child
- Have a family history of depression
- Already had a difficult pregnancy once
- Have insufficient support from friends, family, or partners
- Have experienced or are experiencing domestic abuse
- Have financial problems
- Are going through stressful life situations
- Have a baby with special needs
- Had an unplanned pregnancy
- Are under 20 years of age
Genetics and Postpartum Depression
Studies suggest that having a family history of postpartum depression is one of the causes of postpartum depression. This common subtype of major depressive disorder is more heritable than any other psychiatric condition.
An international team of researchers conducted the largest meta-analyses of genome-wide association studies to study the genetic architecture of postpartum depression. The study established that about 14 percent of the variations observed in cases of postpartum depression may be attributed to common genetic factors. This condition is not associated with only environmental factors but also carries a significant genetic component.
The genetic architecture of PPD was found to be correlated with the genetic architecture of other conditions like major depression, anxiety disorders, bipolar disorder, insomnia, post-traumatic stress disorder, and polycystic ovary syndrome. Therefore, it was discovered that postpartum depression symptoms likely occur because of an interplay between the genes involved in other hormone-related and psychiatric conditions.
Sleep Deprivation and Postpartum Depression
As per evidence, persistent fatigue due to a lack of sleep can increase the risk of postpartum depression for a woman. Sleep quality is affected by sleep deprivation, which makes it difficult for a mother to restore physical energy and agility. Poor sleep can lead to an increase in the symptoms of depression and anxiety.
A single sleep period can not relieve chronic fatigue caused by an imbalance between rest and activity. It is known to affect more than sixty percent of new mothers and may exist due to several factors such as infection, inflammation, anemia, and thyroid dysfunction. The changes in maternal hormones also contribute to postpartum fatigue.
Sleep deprivation in the postpartum period can occur in the form of fragmentation and multiple awakenings after falling asleep, mostly because of the infant’s needs and requirements. Not getting enough sleep can impair the ability of the mother to perform daily tasks with efficiency, for several months after childbirth.
Poor quality sleep is found to elevate depression and anxiety symptoms in mothers at six months postpartum. To prevent chronic fatigue, mothers should implement good Sleep Hygiene as a significant step towards alleviating postpartum depression.
Rebecca had to go through sleep disturbances in the postpartum period. She also remembers being insomniac and struggling to sleep for the recommended number of hours. Implementing sleep hygiene in small yet significant steps would have helped her deal with this situation in a better manner.
Loss of Aspiration and Postpartum Depression
The transition to motherhood can lead to the development of psychological stressors. The drastic changes in a woman’s body, overflowing responsibilities, and how she is perceived in society can cause a lack of self-esteem. Such sudden and overwhelming changes in one’s life can easily cause a loss of aspiration and motivation, strengthening the intensity of postpartum depression symptoms.
In the postpartum period, women are prone to experiencing overwhelming emotions like excitement, anticipation, fulfillment, and happiness, along with the difficult feelings of frustration, confusion, anxiety, guilt, and sadness.
This wide spectrum of emotions and feelings can cause difficulties in maintaining self-esteem, and trigger major loss of aspiration, affecting professional and academic performance, and causing hardships in accomplishment of goals and milestones.
Rebecca recalls experiencing a lack of aspiration and being fearful of the future after having her baby. She almost forgot to spend some fulfilling “me time” and was completely occupied with her child.
Relationship Discord and Postpartum Depression
When a child is born, it has a significant impact on the relationships of the parents. Although this milestone is supposed to bring lots of joy to their lives, shortly after, they might experience emotional distress in the form of parental frustration. These overwhelming feelings can also develop into postpartum depression symptoms not only for the mother but for both parents.
The postpartum depression prevalence in fathers may be less well studied, but it has been established that about ten percent of men go through this condition. Developmentally, the presence of PPD symptoms in mothers may pose risks for the child, but when both parents are affected, the risks increase even more.
The discord between parents and the child is associated with postpartum depression. It can disrupt the bonding between the mother and the child and, sometimes, even lead to abuse. Paternal discord can cause later disorders in children and impact their behavioral development.
What worsens the depressive state of individuals during this phase is that couples may stop doing things they used to enjoy together, such as traveling, going to the gym, seeing friends, and spending evenings out. Sometimes, this disconnection can escalate to the extent that couples even forget to recognize each other as the person they used to love.
The hardest thing that Rebecca had to go through during and after her pregnancy was her relationship discord with her husband. Going through a difficult divorce, she found it difficult to cope in the absence of her partner.
However, she was lucky to have the support of her friends and family, which helped her prevent any severe mental health symptoms. She still believes that the presence of both parents could have been an enriching experience for her daughter and aided in her behavioral development.
While juggling the difficulties of adjusting to the arrival of a newborn, the mother may even find it difficult to maintain her bond with the elder children. The elder children may find it hard to cope with the arrival of a new sibling as it may divide the mother’s attention and make them feel less loved. Such instances of relationship discord contribute to the occurrence and appraisal of postpartum depression, at a time when family members need each other the most.
Sheehan’s Syndrome and Postpartum Depression
First described in 1937, Sheehan’s Syndrome is a postpartum hypopituitarism caused by shock or hypotension because of massive hemorrhage or blood loss during or after delivery. This syndrome may present itself during or after the postpartum period in the form of lactation failure, generalized weakness and debility, cessation of menstrual periods, premature wrinkling of the face and forehead, body hair loss, and dry coarse skin.
It is estimated that Sheehan’s Syndrome occurs in one out of every 1,00,000 births worldwide. Women in developing and under-developed countries lack access to sophisticated medical care, skilled healthcare professionals, and medical resources, which contributes to higher rates of postpartum hemorrhage, and increases this number to five out of 1,00,000 births. It is deemed ‘rare’ in industrialized nations, but the statistics are growing due to the flow of immigrants from developing nations.
The diagnosis of Sheehan’s Syndrome is commonly delayed because of its chronic nature. As it presents itself as a case of multiple hormone deficiencies, it might be differentially diagnosed as hypothyroidism, pituitary tumor, and postpartum depression.
Some patients struggle with achieving the correct diagnosis and are often treated as cases of postpartum depression or major depressive disorder. An incorrect diagnosis leads to the wrong treatment and worsens symptoms, making the patient prone to intensified mental health conditions, including depression.
Clinicians must understand that a combination of Sheehan’s Syndrome and major depressive disorder might exist. However, each case should be appropriately evaluated while recognizing breastfeeding failure and cessation of menstruation as clues for a timely diagnosis.
History of Depression and Postpartum Depression
A previous history of depression and anxiety has been recognized as an important psychological factor contributing to postpartum depression. According to a study that documented about 70,000 births in Sweden between the years 1997 and 2008, women with a history of depression are twenty times more likely to develop postpartum depression as compared to those with no prior depression diagnosis.
Women who have contracted depression earlier are more susceptible to hormonal changes, and can better identify their symptoms. Referring to the research foundations laid by O’Hara MW, it is clear that 23.9% of women who were diagnosed with postpartum depression had experienced depression before. In contrast, only 2.6% of women with no history of psychiatric illness were diagnosed with PPD symptoms.
In line with previous research, this study reveals significant rates of recurring postpartum depression (PPD) among women who have previously experienced PPD. The risk of developing PPD after the birth of a second child was found to be 46.4 times higher (95% CI 31.5–68.4) for women who had been hospitalized for PPD following the birth of their first child. Similarly, women who were treated with antidepressants for PPD after their first child had a 26.9-fold increased risk of experiencing PPD after their second child (95% CI 21.9–33.2).
Anemia and Postpartum Depression
Anemia is a condition in which the body suffers from a lack of red blood cells, or hemoglobin, to carry oxygen to the tissues in the body. During pregnancy, a woman is prone to four kinds of anemia: iron deficiency anemia, anemia of pregnancy, folate deficiency, and vitamin B-12 deficiency. This condition may cause an unfulfilled growth of the baby, due to which it may arrive underweight or early.
Amounting to about 80%, iron deficiency anemia is the most common type of anemia affecting women during pregnancy. Anemia has been recognized as a significant contributing factor to postpartum depression. It is therefore important to pay attention to the nutritional status of women during this period. The prevalence of anemia in pregnant women may be affected by lifestyle, diet, and geographical region.
Anemia can result in adverse pregnancy outcomes, such as preeclampsia, low birth weight, small head circumference and prematurity in the baby, and postpartum depression. As per research, the presence of PPD in anemic women is much higher than in non-anemic women, and there is a significant relationship between anemia and postpartum depression.
High Work Load and Postpartum Depression
A study published on PubMed suggests that higher psychological work demands, lower perceived control over work and family, and lower schedule autonomy elevate the symptoms of postpartum depression. Low job flexibility and a higher workload are other contributors to this condition.
Adapting to the new responsibilities of being a mother, when combined with workplace stress and household responsibilities, especially in an unsupportive environment, can have a daunting effect on women. Such factors can worsen the symptoms of postpartum depression in working women and also have adverse effects on the development of the infant.
Rebecca thinks that her decision to take some time off work after becoming a mother allowed her to rest and recharge. After returning to work, she embraced support from her colleagues, which made it easier for her to integrate work-life balance and restart her career effectively.
Working women may find it hard to manage multiple work commitments and then struggle with the unnecessary guilt of not being a good mother. Mental and social support from peers and colleagues; partners lending a helping hand in household chores; reduced workload in the workplace; maternity leaves; motivation and encouragement to the mother; and equal distribution of responsibilities among the partners are some resolutions to postpartum depression symptoms emerging from poorly managed work-life balance.
Loss of Identity and Postpartum Depression
Experiencing loss of identity is common for new mothers. After having a baby, some parents might feel that being a parent is their only identity. When thoughts of tiredness, worrying and unhappiness extend for too long and it becomes difficult to navigate through a new day, postpartum depression symptoms may elevate.
Loss of identity entails feelings like disrupted professional identity, inability to make money, low-quality social life, less time for leisure activities, and lack of self-confidence. All these characteristics may result in parenting issues and a lack of bonding with the baby.
In most cases, mothers stop pursuing activities they once loved, for example, seeing friends, taking long showers, embracing quality time with their partners, and engaging in hobbies. They may start to feel like they have no time for themselves anymore. Some effective solutions for dealing with loss of identity include:
- Thinking of all the positive changes after childbirth
- Having breaks from the busy routine
- Making time for self-care
- Ignoring comparison with other parents
- Self-acceptance
Difficult Pregnancy and Postpartum Depression
Difficulties in pregnancy may occur because of concerns about the mother’s health, the fetus’s health, or both. Even healthy women may face difficult pregnancies and go through a hard time. Complications may take the form of high blood pressure, gestational diabetes, infections, preterm labor, stillbirth, preeclampsia, etc. Mothers who do not receive enough and timely prenatal care are prone to developing such pregnancy complications, which may significantly contribute to the elevation of postpartum depression.
High-risk pregnancies may occur because of a pre-existing medical condition before pregnancy, or conditions that develop during the pregnancy. Factors that may contribute to hard pregnancies include:
- Too young age (less than 20 or more than 35)
- Lifestyle choices such as consuming alcohol, cigarettes, or drugs
- Chronic health conditions such as high blood pressure, diabetes, obesity, thyroid, or infections
- Pregnancy complications such as the unusual location of the placenta, low fetal growth, and Rh sensitization
- Pregnancy with multiple babies
- Problematic pregnancy history, such as miscarriage or stillbirth
Experiencing a pregnancy with high-risk factors can be anxiety-inducing and lead to concerns about the well-being of the baby. Taking proactive steps to promote a healthy pregnancy and maintaining open communication with the healthcare provider throughout the pregnancy, addressing any inquiries, or seeking support as needed are some important steps.
Additionally, it is also advisable to consult with a healthcare professional post-pregnancy to discuss potential impacts on long-term health resulting from medical conditions during pregnancy.
Hormonal Imbalance and Postpartum Depression
Studies indicate that the rapid changes in reproductive hormones like estradiol and progesterone before and after childbirth may play a role. While several studies, both in humans and animals, have indicated a link between changes in hormone levels and PPD, other studies have failed to find any association between hormone concentrations and PPD symptoms.
For instance, research examining the differences in ovarian hormone levels and depressive symptoms during the postpartum period has not shown a direct correlation between absolute estrogen and progesterone concentrations and PPD.
However, studies that have utilized estradiol treatment have successfully alleviated depressive symptoms, and animal studies have shown that withdrawal of estradiol and progesterone can induce depression-like behavior.
Reproductive hormones have a significant role in various aspects such as basic emotion processing, arousal, cognition, and motivation. Consequently, they could indirectly contribute to postpartum depression by influencing psychological and social risk factors. Interestingly, these hormones also regulate the biological systems involved in major depression, suggesting a direct impact on a woman’s risk for PPD.
Thyroid hormones have been suggested as a potential biomarker for PPD due to the presumed connection between thyroid dysfunction and major depression. It is known that thyroid dysfunction is associated with pregnancy and may potentially contribute to PPD in certain women.
Nutritional Deficiency and Postpartum Depression
Malnutrition, or deficiencies of certain nutrients like B and D Vitamins, n-3 polyunsaturated fatty acids (PUFA), folate, trace minerals, iron, antioxidants, etc. can increase the risk of postpartum depression. Lactation and pregnancy place additional demands on the body of a new mother, due to which nutritional deficiencies arise more easily during this time and pave the way for depression symptoms.
Lack of Vitamin D and Postpartum Depression
Investigations are currently underway to determine if low levels of vitamin D could potentially increase the risk of postpartum depression. This is because vitamin D acts as a neuroactive hormone, playing a crucial role in the nervous system rather than the endocrine system. Its main function is to connect sensory stimuli with the release of hormones, resulting in a hormonal response.
By regulating neurotransmitters such as adrenaline, norepinephrine, dopamine, and serotonin, vitamin D contributes to this process. Any disturbances in these neurotransmitters and hormones have been linked to the development of depressive symptoms.
Lack of Omega-3 Fatty Acids and Postpartum Depression
Omega-3 fatty acids have also been connected to PPD. Docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) are two types of omega-3 fatty acids that are well-known for their positive effects on heart health, but they also play a crucial role in the development of the human brain and the regulation of neurotransmitters.
Increased levels of DHA and EPA are associated with improved sensitivity of serotonin receptors, achieved by increasing the fluidity of the receptor cell membrane. Furthermore, it is hypothesized that omega-3 fatty acids may reduce neuroinflammatory processes, which have been linked to the onset of depression.
In the United States, it has been reported that many people have insufficient levels of omega-3 fatty acids because their diets do not provide enough of these nutrients. The typical American diet consists mainly of fast food, which lacks the necessary nutrients and fails to meet recommended nutritional guidelines.
Pregnant women are particularly vulnerable to the negative effects of low omega-3 fatty acids. This is because the increased blood supply required for fetal oxygen needs leads to a natural decrease in levels of DHA and EPA. In addition, the body prioritizes the growth and development of the fetus by redirecting blood and nutrients, putting pregnant women at a higher risk of developing nutritional deficiencies and thus, postpartum depression.
Dealing with postpartum depression (PPD) can be challenging for both the mother and the child. It poses a threat to the mother’s well-being and the proper development of the child. Women experiencing PPD often struggle to maintain regular breastfeeding due to their depressive symptoms.
PPD complicates the mother-child relationship, leading to issues such as poor cognitive functioning, aggressive behavior, excessive crying, emotional instability, and sleep problems in infants and adolescents. PPD is associated with negative thoughts, substance abuse, postpartum psychosis, hallucinations, confusion, mood swings, paranoia, impaired judgment, disorganized behavior, loss of appetite, and insomnia in mothers.
It hampers a woman’s ability to interact and socialize even within her own family, making her feel like an inadequate mother and preventing her from enjoying activities and hobbies. Women with PPD are also at risk of infanticide and suicide, as well as developing serious mental disorders like bipolar disorder.
“It is crucial for women to seek help for postpartum depression in a world where people are overly invalidating. Women should know that going through PPD is normal and sometimes inevitable”, says Rebecca.
She suggests seeing an Online Psychiatrist for postpartum depression, as it is economical, involves less hassle, and is more accessible.
Gaba Telepsychiatry’s psychiatrists strive to provide a comprehensive approach to psychiatric care without compromising evidence-based medicine. Our online psychiatrists take into account a variety of factors, including genetics, developmental, trauma, nutritional factors, hormones, career difficulties, relationship difficulties, coping skills, concurrent medical illness, head injury, medication side effects, and more.
Visit https://gabapsychiatrist.com/postpartum-depression-treatment to find out more!